Case Report - (2022) Volume 5, Issue 4
Negative Pressure Pulmonary Edema: A Case Report
Mohammad Mahbube Mustafa1*, Kuenza P Wangmo1, Kamal Ahmed Chowdhury2, Sonam Tobgay3, Kuenzang Wangden4 and Md. Rafiqul Alam Talukder52Junior Consultant, Department of Anesthesiology, Sir Salimullah Medical College & Mitford Hospital, , Bangladesh
3Resident of Anesthesiology, Jigme Dorji Wangchuk National Referral Hospital, Thimphu, Bhutan
Resident of Anesthesiology, Jigme Dorji Wangchuk National Referral Hospital, Thimphu, Bhutan
4Assistant Professor (Anaesthesia), Sheikh Hasina Medical College, Tangail, Bangladesh
Received: Nov 21, 2022, Manuscript No. AMDHS-22-80514; Editor assigned: Nov 22, 2022, Pre QC No. AMDHS-22-80514 (PQ); Reviewed: Nov 23, 2022, QC No. AMDHS-22-80514 (Q); Revised: Nov 23, 2022, Manuscript No. AMDHS-22-80514 (R); Published: Dec 01, 2022, DOI: 10.5530/amdhs.2022.4.10
Abstract
Negative pressure pulmonary edema is an uncommon complication of the extubation of the endotracheal tube. An increase in intrathoracic pressure and negative pressure of the lung caused by acute laryngeal spasm results from acute upper respiratory obstruction causing life-threatening pulmonary edema by alveolar-capillary damage is called negative pressure pulmonary edema. We here describe 37-years old male case the preoperative diagnosis of Chronic Bilateral nasal Obstruction associated with headache undergoing Functional Endoscopic Sinus Surgery (FESS) with septoplasty caused negative pressure pulmonary edema while extubation. With the immediate treatment, the patient was discharged without any abnormalities.
https://aermech.com https://world-oceans.org https://lline.net https://apecu.org https://febayder.com https://johnbirch.org
Keywords
Extubation, Laryngospasm, Pulmonary Edema
Introduction
Negative Pressure Pulmonary Edema (NPPE) is noncardiogenic pulmonary edema, induce due to an increase in intrathoracic pressure and negative pressure of the lung as a result of acute laryngeal spasm during extubation. NPPE is a life-threatening condition during the extubation after general anesthesia. The prevalence of NPPE occurs in 0.05% to 0.1% [1]. It usually occurs in young healthy patients and during extubation due to which it is also called “post-extubation pulmonary edema” [2]. We here discuss a case of 37 years old male case with a preoperative diagnosis Chronic Bilateral nasal Obstruction associated with headache occurring NPPE during extubation.
Case Presentation
A 37-years old man presented to the Jigme Dorji Wangchuk National Referral Hospital (JDWNRH), Thimphu, Bhutan with complaints of chronic bilateral nasal obstruction associated with headache. Normal past medical history without any comorbidity except, he had hypertension well controlled with medication. There was no history of any past surgery, trauma, allergies, smoking, drug addiction, and infectious diseases. No specific family history was found. On physical examination, there was no abnormality in any system. All the other preoperative assessments including laboratory examinations, imaging examinations, and physical examinations were under normal range.
He was scheduled for Functional Endoscopic Sinus Surgery (FESS) with septoplasty with general anesthesia. The patient was fasted for 12 hours. American Society of Anesthesiologists (ASA) of degree II with height 177 cm, weight 74 kg, BMI 23.6 kg/m² was reported. His Mallampati grade was II degree. Preoperative vital signs were stable with blood pressure of 140/84 mmHg, heart rate 82 bpm, and SpO2 100%.
For Anesthesia induction drugs used Fentanyl l00 μg, Thiopental Sodium 200 mg, midazolam 2 mg and succinylcholine 100 mg then Atracurium 30 mg to maintain muscle relaxant. Operation start time 10:10 am. His vital signs during the operation were stable. EtCO2 was under normal range. Total operation duration was 2 hours. A total of 1500 mL of ringer lactate solution was administered during the surgery, the urine output was approximately 200 mL, and blood loss was less than 20 mL.
Extubation was done at 12:20 am with self-spontaneous breathing observation, tidal volume of 500 L, and when he obeyed the command of opening eyes. Right after extubation patient had breathing difficulties; with mask ventilation positive pressure SpO2 was 88%. But it was ineffective, the further deterioration of SpO2 was observed with 75% to 60%. Pink frothy sputum was found around the mouth and during suction. Atropine 0.5 mg, neostigmine 1 mg was given. Bilateral pulmonary rales were auscultated at the time. With failure to raise in SpO2 patient was reintubated at 12:37 am with sevoflurance 1.8% continuous inhalation, fursemide 20 mg, hydrocortisone 100 mg, aminophyline 0.125 mg, dexmedetomide 20 ug, and dexamethasone 8 mg was given. The SpO2 gradually returned to normal and the patient was taken to the HDU with an endotracheal tube. In HDU physical warmer, atracurium 10 mg was used with continuous observation. The blood gas analysis and chest X-ray was taken immediately. The vital signs and urine output was normal in HDU. After 12 hours of observation, the patient was extubated successfully. The patient was sent to the ward without any discomfort and abnormalities.
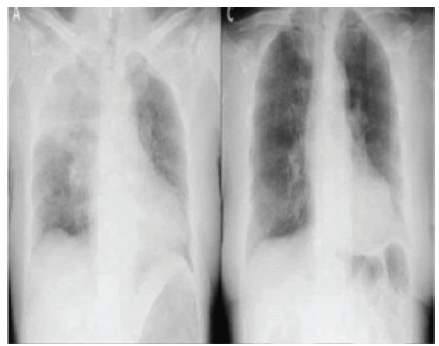
A chest X-ray is taken when the patient was sent to HDU and after 8 hours (FIGURE 1 A, B). The chest X-ray at the left side taken when the patient was sent to HDU showed bilateral diffuse, bilateral, hazy, interstitial opacity, pulmonary infiltration throughout both lungs. The chest X-ray at the right side taken after 8 hours patient was sent to HDU showed resolution of the process.
ABG at left side taken when the patient was sent to PACU and right side was taken after 8 hours showed improved SpO2 (TABLE 1).
| Parameters | ABG at PACU | ABG after 4 hours |
|---|---|---|
| Base excess (BE) | 1.0 mmol/L | 1.0 mmol/L |
| Calcium (Ca) | 1.10 mmol/L | 1.10 mmol/L |
| Chlorine (Cl) | 101 mEq/L | 102 mEq/L |
| Glucose (Glu) | 7.3 mmol/L | 7 mmol/L |
| Haemoglobin (Hb) | 123 g/dl | 120 g/dl |
| Bicarbonate (HCO3) | 24 mEq/L | 23.3 mEq/L |
| Haematocrit (Hct) | 36% | 37% |
| Potassium (K) | 3.86 mEq/L | 3.96 mEq/L |
| Sodium (Na+) | 140 mEq/L | 143 mEq/L |
| Partial pressure of carbondioxide (PaCO2) | 44 mmHg | 42 mmHg |
| Acidity (pH) | 7.32 | 7.35 |
| Partial pressure of oxygen (PaO2) | 60 mmHg | 100 mmHg |
| Oxygen saturation (SPO2) | 70% | 97.60% |
After the patient was sent to ward ABG report was found under normal ranges, timely vitals, and urine output observation was done. The blood gas analysis (ABG) and chest X-ray was taken regularly with no suspicion and abnormalities. Then the patient was discharged without any abnormalities after 2 days.
Discussion
Negative pressure pulmonary edema is an uncommon complication of the extubation of the endotracheal tube. NPPE has been reported mainly by anesthetists as a consequence of postoperative laryngospasm [3]. The pathophysiology of NPPE begins with acute laryngeal spasm leading to severe upper airway obstruction. Intrathoracic pressure during acute upper airway obstruction is (> -100 cm H2 O) whereas normal inspiratory chest pressure is (-2 cm to -5 cm H2 O). The absolute value of intrathoracic transpulmonary negative pressure leads to the reduce of alveolar-capillary membrane pressure causing disruption of capillary barrier and alveolar epithelial barrier. All these cause exudation of blood vessels, which makes the red blood cells leak into the alveoli and causes significant lung or bronchial bleeding. These changes lead to red blood cell filtration into the lung and pulmonary edema [4]. The increase in pulmonary blood volume occurs due to the increase in systemic arterial pressure secondary to the release of norepinephrine in response to hypoxia, hypercapnia, and agitation. Frothy pink pulmonary secretions is one of the most important syndrome to diagnose NPPE during extubation and before making the diagnosis of NPPE, other causes of pulmonary edema particularly those requiring a rapid intervention (fluid maldistribution, anaphylaxis, and cardiogenic pulmonary edema), must be considered [5]. The main diagnosis is done by incidence and symptoms, chest radiograph for pulmonary edema, and measure of pulmonary edema fluid/plasma protein ration. With proper treatment, NPPE can rapidly dissipate. The most important treatments include re-establishment of the airway by relief airway obstruction. Adequate oxygenation should be given, encourage the patient to cough after extubation. Application of positive airway pressure via face mask or LMA or Endotracheal intubation with ventilator support. Although NPPE does not result from fluid overload, it is recommended gentle diuresis using low-dose furosemide [6]. The clinical syndromes can usually improve after 12 hours to 24 hours [7]. In our case, the symptoms were improved within 12 hours without any abnormalities. Patients with NPPE history should be kept in mind and prevention methods can be performed accordingly. It is also believed that the incidence of NPPE is higher than that found in the literature due to the fact that the cases are poorly diagnosed and, in many cases, confused with pulmonary edema due to fluid overload, aspiration pneumonitis and bronchospasm [8].
Conclusions
Functional Endoscopic Sinus Surgery (FESS) with septoplasty caused negative pressure pulmonary edema while extubation. With the immediate treatment, the patient was discharged without any abnormalities.
References
- Liu RZ, Wang J, Zhao GQ, Su ZB. Negative pressure pulmonary edema after general anesthesia: a case report and literature review. Medicine. 98(17), e15389 (2019).
- Pathak V, Rendon IH, Ciubotaru RL. Recurrent negative pressure pulmonary edema. Clin Med Res. 9(2), 88-91 (2011).
- Bhaskar B, John JF. Negative pressure pulmonary edema revisited: Pathophysiology and review of management. Saudi J Anaesth. 5(3), 308-313 (2011).
- Lemyze M, Mallat J. Understanding negative pressure pulmonary edema. Intensive Care Med. 40(8), 1140-1143 (2014).
- Krodel DJ, Bittner EA, Abdulnour R, Brown R, Eikermann M. Case scenario: acute postoperative negative pressure pulmonary edema. Anesthesiology. 113, 200-207 (2010).
- Bhattacharya M, Kallet RH, Ware LB, Matthay MA. Negative-pressure pulmonary edema. Chest. 150(4), 927-933 (2016).
- Xiong J, Sun YX. Negative pressure pulmonary edema: A case report. BMC Anesthesiol. 19(1), 1-6 (2019).
- Albergaria VF, Soares CM, Araujo RDM, Mendonca WLD. Negative- pressure pulmonary edema after transsphenoidal hypophysectomy: Case Report. Rev Bras Anesthesiol. 58(4), 391-396 (2008).